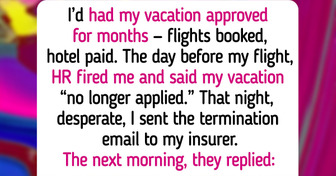
HR Fired Me Right Before My Vacation, So I Used It Against Them

Sleep apnea may appear to be just a case of snoring, but it is more than that. It impacts not only your sleep but also your overall quality of life. So, how can you determine if you have sleep apnea? There are signs to be aware of, and it’s essential to pay attention to them as they may indicate larger health issues.
CONTENT IS PROVIDED FOR INFORMATIONAL PURPOSES ONLY AND IS NOT INTENDED AS A SUBSTITUTE OF MEDICAL ADVICE. SEEK GUIDANCE OF YOUR DOCTOR REGARDING YOUR HEALTH AND MEDICAL CONDITIONS.
Sleep apnea is a serious disorder marked by repeated breathing interruptions during sleep. Common symptoms include loud snoring and daytime fatigue, even after a full night's rest. Untreated sleep apnea can affect daily functioning and lead to severe health risks, including diabetes and heart issues.
Statistics indicate that up to 30 million Americans may have sleep apnea, often without diagnosis. Being aware of its symptoms helps determine when to see a doctor.
There are three types of sleep apnea:
Here are the symptoms of sleep apnea, both common and uncommon.
If you or a loved one experience these symptoms, consider consulting a healthcare professional for evaluation.
Obstructive sleep apnea can stem from various conditions, with some risk factors being changeable and others not. According to the National Heart, Lung, and Blood Institute, key factors include:
Untreated sleep apnea can lead to serious health issues, including type 2 diabetes, strokes, and heart attacks. Jonathan Jun, M.D., notes that obesity greatly increases these risks, though sleep apnea can affect individuals of any weight. Weight loss is critical for prevention and treatment, especially for those accumulating fat in the neck and abdomen.
Women, particularly as they age, should be aware of shifting weight patterns that could lead to sleep apnea.

Sleep apnea can range from mild to severe, assessed using the apnea-hypopnea index (AHI), which measures breathing pauses during sleep.
Severe: AHI > 30 (over 30 episodes per hour)
Moderate: AHI 15-30
Mild: AHI 5-15
Addressing sleep apnea is crucial to prevent long-term health effects.
The need for treatment for sleep apnea depends on its severity and the presence of symptoms like daytime sleepiness or other health issues. For those at risk for heart disease, treatment may be recommended even for mild cases. Severe sleep apnea may require treatment regardless of symptoms.
The primary treatment is the CPAP machine, which provides humidified air through a mask to keep the throat open during sleep, preventing breathing interruptions. Regular use of a CPAP has been shown to lower blood pressure and improve daytime alertness and quality of life.
If you suspect sleep apnea, consult a healthcare provider. A sleep specialist can conduct tests to monitor breathing and oxygen levels during sleep, either in a lab or with a portable kit.
Making specific lifestyle adjustments can help mitigate the risks of sleep apnea:
If you or your partner observe symptoms of sleep apnea, consult a healthcare provider. They may review your health history, recommend a sleep study, and discuss lifestyle changes or CPAP treatment.
Regular follow-ups are essential to evaluate treatment effectiveness and address any new sleep issues.
When it comes to health, there’s no such thing as being overly cautious, and it’s essential to prioritize your well-being at all times.